

A procedure where the embryologist directly injects a single sperm into the egg, causing fertilization. This may be helpful in cases where there is poor quality sperm from the male partner, or where there is an issue with the egg where fertilization can’t occur due to changes in the membranes surrounding the egg.
ICSI is an acronym for intracytoplasmic sperm injection. IVF with ICSI involves the use of specialized micromanipulation tools and equipment and inverted microscopes that enable embryologists to select and then pick up individual sperms in a tiny specially designed hollow ICSI needle. Then the needle is carefully advanced through the outer shell of the egg and egg membrane and the sperm is then injected into the inner part (cytoplasm) of the egg. This will usually result in normal fertilization in approximately 70-85% of eggs injected with viable sperm. First, the woman must be stimulated with medications and have an egg retrieval procedure so that we can obtain several eggs in order to attempt in vitro fertilization and ICSI.
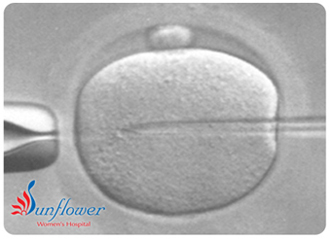
Using micromanipulation technology, ICSI allows fertility specialists to fertilize an egg using just one sperm. While it is preferred to use sperm from a semen sample, specialists can retrieve sperm from the testicles if it is necessary. This process bypasses the conventional IVF methods of fertilization, thereby ensuring that fertilization has taken place. The fertilized eggs are then left to culture for a few days before being transferred back to the woman’s uterus. ICSI is always used alongside IVF.