

IVF is basically a safe procedure. The most common complications associated with IVF treatment are the failure of treatment, problems experienced as a consequence of ovarian stimulation, the risk of multiple pregnancy, the risks associated with egg collection and the possibility of ectopic pregnancy.
This is the most common complication of treatment. The likely reasons for this failure are cancelled cycles (approximately 10% of treatment cycles will be abandoned before egg collection), failure to collect eggs (about 1%), failure of fertilization (about 5%), and failure of implantation (this could be due to defective embryo or endometrium, or poor synchronization).
The IVF (in-vitro fertilization) procedure is considered by some, to be one of the most stressful infertility treatments. Failure of treatment can result in emotional strain, psychological stress and depression. Some couples may require psychological counseling.
There is no drug that is absolutely safe and completely free of side effects. There are potential problems, which may occur and include: side effects of fertility drugs, ovarian hyperstimulation syndrome (OHSS), multiple pregnancy, adnexal torsion (ovarian twisting) and the risk of ovarian cancer.
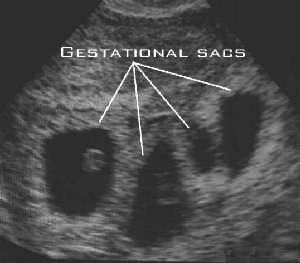
Although the prospect of twin or triplets may seem attractive to some couples, high order of multiple pregnancies is associated with increased risks of maternal and fetal complications. In addition, multiple pregnancies place enormous strains for the parents including financial difficulties, emotional distress and physical exhaustion.
If all twins, triplets, and quads were born as healthy as singletons there would not be any concerns. Unfortunately, multiple pregnancies have much higher risks than singletons for the fetuses and also for the mother. The risk of these complications arising must be balanced against the number of embryos transferred and the corresponding increase in success rate.
This is the most serious complication of IVF. Any patient undergoing ovulation induction is at risk of developing OHSS, although some more than others.
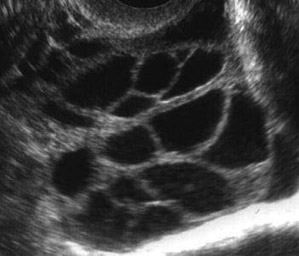
Ovarian hyperstimulation syndrome may be classified as mild, moderate or severe by symptoms and signs. the worst cases seem tends to be associated with pregnancy. Severe OHSS is a life threatening complication following ovarian stimulation.
The symptoms usually begin 4-5 days after the egg collection. The majority of women have a mild or moderate form of the syndrome and invariably resolve within a few days unless pregnancy occurs, that may delay recovery. Patient may complain of pain, a bloated feeling and mild abdominal swelling. In a small proportion of women, the degree of discomfort can be quite pronounced.
In some cases cysts appear in the ovaries (ovarian cysts) and fluid may collect in the abdominal cavity causing discomfort.
Very rarely the ovarian hyperstimulation is severe and the ovaries are very swollen. The woman will feel ill, with nausea and vomiting, abdominal pain. Fluid accumulates in the abdominal cavity and chest, causing abdominal swelling and shortness of breath. Reduction in the amount of urine produced. These complications require urgent hospital admission to restore the fluid and electrolyte balance, monitor progress, control pain and in some very serious cases, termination of pregnancy.
Complications associated with severe OHHS include blood clotting disorders, kidney damage and twisted ovary (ovarian torsion).
Despite careful monitoring, up to 33% of IVF treatment have been reported to be associated with mild forms of OHSS. Severe OHSS has been reported in 3-8% of IVF cycles
Over response to fertility drugs. Cause is unknown. But, women at risk of developing OHHS include.
As with any surgical procedure, there are potential risks associated with egg collection. Such risks depend on whether the egg collection is performed by vaginal ultrasound or laparoscopy.
Mild to moderate discomfort.
Laparoscopic egg collection has similar complications to those described above, but the risk of injury to internal organs is higher than after ultrasound scan. In addition, there is risk of complications associated with the use of a general anesthesia, although this is rare in healthy women..
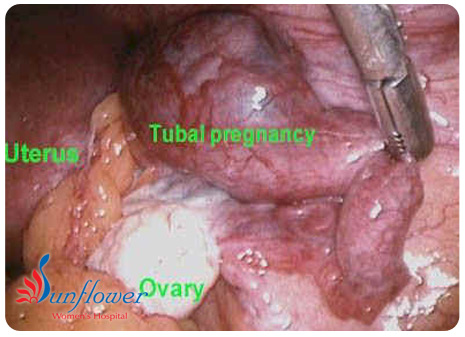
One of the potential risks of fertility treatments such as In-Vitro Fertilisation (IVF) and Intrauterine Insemination (IUI) is the increased chance of ectopic pregnancy. Ectopic pregnancy occurs when a woman’s egg is fertilised by her partner’s sperm and the resulting embryo implants somewhere outside the woman’s womb. When an embryo grows outside the womb, a potentially life-threatening situation is created for both mother and foetus. Health statistics show that approximately 1 % of all pregnancies are ectopic. According to NHS statistics, in 95 % of ectopic pregnancies, the embryo remains in the fallopian tube – although ectopic pregnancy can occur in the cervix (the neck of the womb), the ovary and the abdominal cavity. The danger is that the affected organ will rupture and cause severe bleeding. Generally, an embryo cannot survive an ectopic pregnancy and therefore treatment nearly always requires the removal of the embryo.
During IVF treatment, a woman’s eggs are removed directly from her ovaries and are fertilised with her partner’s sperm outside her body (in a laboratory). The resulting embryos are then inserted directly into her womb. Given that most ectopic pregnancies occur when a fertilised egg gets stuck in the fallopian tube,
how IVF could possibly increase the chances of ectopic pregnancy,
since IVF “bypasses” the fallopian tubes altogether. Fertility specialists believe that ectopic pregnancy may occur if, when the embryos are transferred to the womb, they are placed too high in the womb cavity. The embryos then have a greater chance of “wandering” and implanting themselves in places where they are not supposed to be, such as the fallopian tubes. Embryos could also make their way into the fallopian tubes if they are injected into the womb with too much force.