



In the past, men who failed to have any sperm present in their semen would not have been able to conceive a biological child. Instead, couples suffering from this type of male factor infertility would have had to rely on a sperm donor in order to conceive a child. Nowadays, though, a variety of techniques exist that can be used to collect sperm directly from the testicles, which can then be used in ICSI.
Our goal at the Center for Male Reproductive Medicine is to provide the safest, most effective patient care and to collect as much good quality sperm as possible to minimize the need for future multiple surgeries.
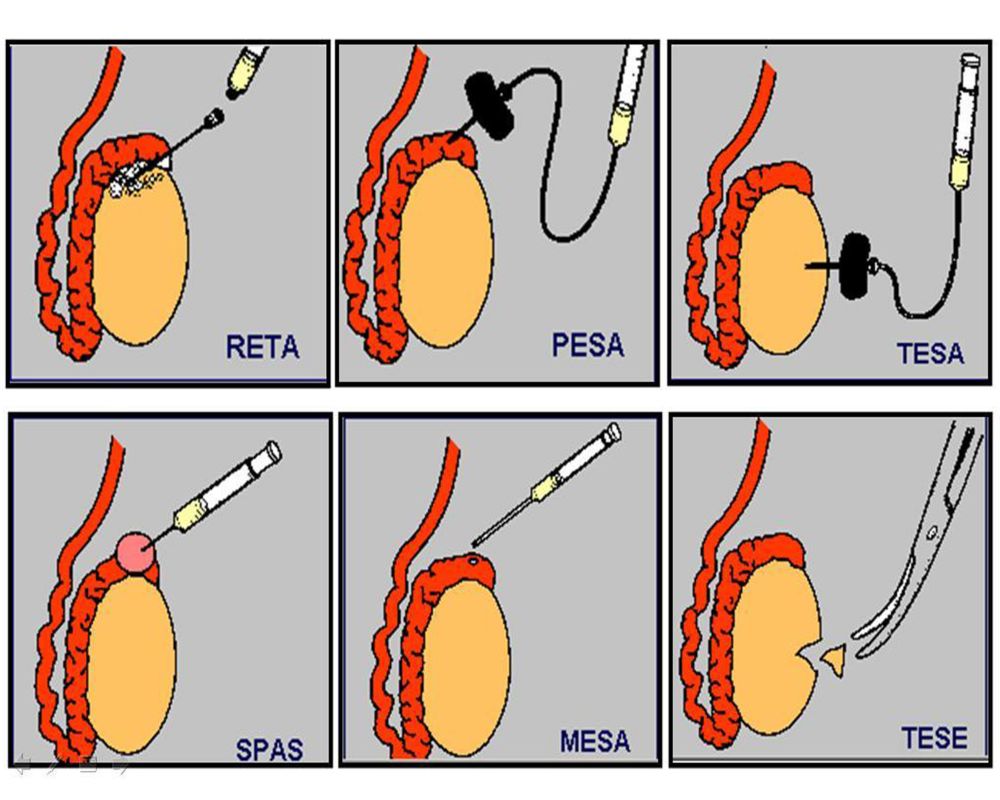
Surgical sperm retrieval (SSR) is actually an umbrella term that refers to a variety of different techniques that can be used to obtain sperm from a man. Because there is very little, if any, sperm in the man’s ejaculate, it is necessary to extract sperm directly from the vas deferens, epididymis or the testicles.
Surgical sperm retrieval is not for every man. In general, those men who are experiencing infertility due to one of the following reasons may be able to use SSR in combination with ICSI and IVF in order to produce a pregnancy:
There are a variety of methods used to surgically remove sperm from within the genital tract. Which form of SSR is best for you will depend upon the reason why sperm is absent from your ejaculateThey are generally classified as being minor procedures and often require no more than local anesthetic and a recovery period of only a few days.
Percutaneous sperm aspiration (PESA) is often the first course of treatment when no sperm is found in a man’s semen, as it does not require any surgical cuts. It is a fairly short procedure, taking no more than 20 minutes to complete and requires only local anesthetic. During PESA, a needle is inserted through the scrotum into the epididymis and is used to remove the liquid inside. Because doctors are looking to collect between 10 and 20 million sperm, in some cases, multiple aspirations in one or both of the testicles are necessary. Since sperm removed from the epididymis are not fully matured yet, it is necessary to use ICSI to fertilize an egg. Men with CAVD or who have scar tissue in their vas deferens are the most suited to this procedure.
This type of SSR is commonly used in men whose vas deferens is blocked or who have had a vasectomy within the last five years. This simple procedure requires the use of local anesthetic and is the only type of SSR that is able to retrieve mature sperm. During the procedure, a needle is inserted into the vas deferens, possibly through a small incision made in the scrotum, extracting the fluid inside. The vas deferens and epididymis are then massaged to produce additional liquid, which will also be removed. Extracted sperm is then prepared for IVF. As this procedure removes sperm that has passed through the epididymis, and is therefore considered to be mature, sperm retrieved through vasal aspiration can be cryopreserved for use in future treatments and does not necessarily need to be used in conjunction with ICSI.
This procedure is very similar to PESA except that in MESA, a tiny incision is made through the scrotum and into the epididymis. Fluid from the epididymal tube is then drained out and analyzed for sperm. This type of microsurgical treatment is generally recommended for men who do not have a vas deferens or have scar tissue in their vas deferens. MESA is usually done under general anesthetic.
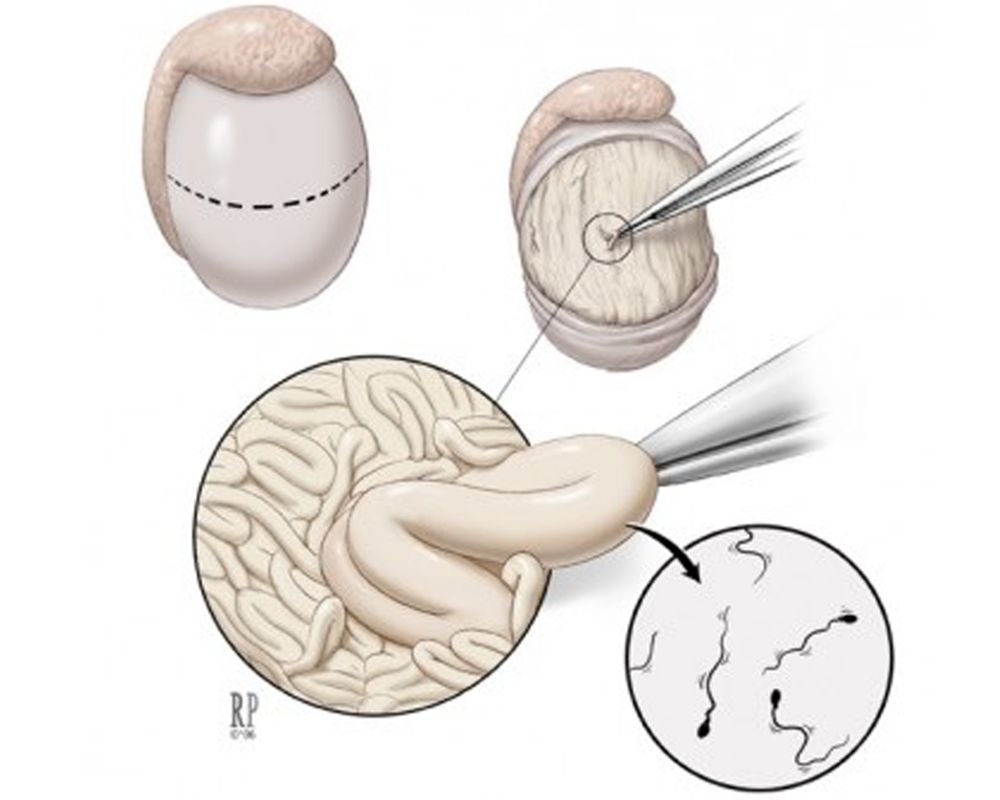
This type of SSR is reserved for men who have a blockage in their epididymis, close to the testicles, thereby preventing sperm from entering into the epididymis. It can also be used in men who have a blockage in the testicles or produce so little sperm that none of it reaches the ejaculate. In testicular sperm extraction (TESE), immature sperm is collected through a testicular biopsy, a process that requires the removal of a small amount of testicular tissue. Local anesthetic is usually given before the surgeon makes a small incision in the testicles to remove the tissue. A similar procedure, known as testicular sperm aspiration (TESA), also removes sperm directly from the testicles. However, in this procedure, no incision is made and instead a needle is inserted directly into the testicles in order to collect the sperm. Because sperm collected from the testicles are immature, it is necessary to use ICSI in order to fertilize an egg. Several studies have demonstrated that TESE is superior to TESA in all regards. The potential for complications is higher with this technique than with TESE (open biopsy) for two important reasons. TESA is a blind needle stick and bleeding can not be stopped when it is accidentally encountered. The needle is larger in diameter than the intratesticular artery and can sever the artery, potentially cutting off testicular blood supply. The testicle may shrink and die. It is because of these reasons that we rarely offer TESA to our patients. Open biopsy (TESE) is more effective and potentially safer than needle biopsy (TESA) and is our technique of choice for obtaining testicular sperm for men with non-obstructive azoospermia.
Finding success with surgical sperm retrieval depends heavily upon the SSR method you undergo. PESA has the highest rate of retrieval associated with it, at 80% to 90%, while TESE tends to be much lower, with only 60% of patients having sperm retrieved. As all of these methods require the use of IVF, and often ICSI as well, the chances of pregnancy tend to however between 20% and 30%, again dependant upon the method of SSR used.
Another concern for many with SSR is the fact that, often, immature sperm are retrieved. Because TESE removes sperm that have never passed through the epididymis, some experts are concerned about using cells that are still evolving to achieve pregnancy. In some instances, spermatids (round cells that have yet to develop into sperm with tails) may be removed through TESE. Although spermatids can be used with ICSI to cause pregnancy, it is still thought of as an experimental treatment.
Before deciding on SSR, discuss all the pros and cons of these procedure with your fertility doctor. It is also a good idea to come up with a back-up plan in case it is not possible to remove enough sperm through SSR.