

Follicle stimulating hormone (FSH) is one of the most important hormones involved in the natural menstrual cycle as well as in pharmacological (drug-induced) stimulation of the ovaries. It is the main hormone involved in producing mature eggs in the ovaries.
FSH is the same hormone that is contained in the injectable gonadotropins which are used to produce multiple eggs for infertility treatment.
Women in menopause usually have high FSH hormone levels that are above 40 mIU/ml. As women approach menopause their baseline FSH levels (day 3 of their cycle) will tend to gradually increase over the years.
By measuring a woman’s baseline FSH on day 3 of the cycle (we do it on day 2, 3, or 4), we get an indication as to whether she has normal “ovarian reserve”.
Therefore, if the baseline FSH is elevated the ovarian reserve (how many eggs are left) is reduced (sometimes the egg quality is also reduced).
A blood estradiol level on day 3 (we do it on any day between days 2 and 4) of the menstrual cycle is a way to potentially discover some of those women with a normal day 3 FSH that may in fact have decreased egg quantity and quality.
What we want on day three is a low FSH level in conjunction with a low estradiol level. If the FSH is normal but the estradiol level is elevated, the elevated estradiol will often be artificially “suppressing” the FSH level down to the normal range.
We like to see the day 3 estradiol less than about 80. In our clinic, levels of 80-100 are borderline, and over 100 are abnormal. We repeat borderline or abnormal results in another menstrual cycle to try to get a “true” FSH..
Antral follicles are small follicles (about 2-8 mm in diameter) that we can see – and measure and count – with ultrasound. Antral follicles are also referred to as resting follicles.
Vaginal ultrasound is the best way to accurately assess and count these small structures. In my opinion, the antral follicle counts (in conjunction with female age) are by far the best tool that we currently have for estimating ovarian reserve and/or chances for pregnancy with in vitro fertilization.
As women age, they have less eggs (primordial follicles) remaining, therefore they have fewer antral follicles on ultrasound.
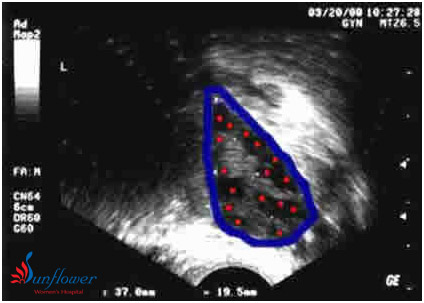
Ultrasound image of an ovary at the beginning of a menstrual cycle. No medications are being given. The ovary is outlined in blue. There are numerous antral follicles visible – marked with red spots. 16 are seen in this image, this ovary had a total of 35 antrals (only 1 plane is shown above) This is a polycystic ovary, with a high antral count and volume (ovary = 37 by 19.5mm) This woman had irregular periods and was a “high responder” to injectable FSH medication.
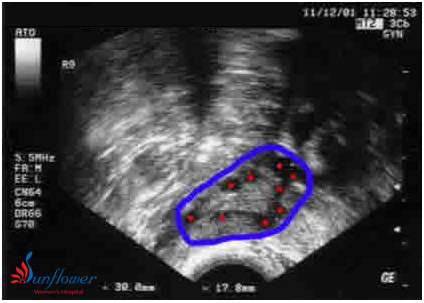
Ultrasound image of an ovary at the beginning of a menstrual cycle. No medications are being given. The ovary is outlined in blue. 9 antral follicles are seen – marked with red spots The ovary has normal volume (cursors measuring ovary = 30 by 17.8mm) This woman had regular periods and a normal response to injectable FSH drugs

An ovary is outlined in blue and is small (low volume) with only 1 antral follicle. Her other ovary had only 2 antral follicles. She had regular periods and a normal day 3 FSH test. Attempts to stimulate her ovaries for IVF were not successful
There is not a perfect answer to this question. This means that if we had several different trained ultrasonographers do an antral count on a woman, they would not all get exactly the same result. 3-5 antral follicles would be indicative of good ovarian
Attempts to do IVF are sometimes “cancelled” when the ovaries respond very poorly to the stimulation meds because success rates are very low with less than 3 mature follicles.
There are no absolute and accepted cutoffs for defining “low”, “normal”, or “high-responders”. However, here are some general guidelines:
Low responder:- When stimulated aggressively with injectable FSH will develop less than 5 mature follicles - often requiring high doses of the medications. Some women will only develop 1 or 2 mature follicles - even on very high doses of the medications. These women are not good candidates for IVF using their own eggs - but are good candidates for in vitro fertilization with donor eggs.
“Normal” or “average” responder: When stimulated aggressively with injectable FSH will develop 5-8 mature follicles as well as several smaller ones.
High responder: When stimulated aggressively with injectables will develop about 8 or more mature follicles as well as many small and medium-sized follicles. These women usually respond briskly to lower doses of medications. They are at higher risk for ovarian hyperstimulation syndrome.
AMH, or anti-mullerian hormone is a substance that is produced by granulosa cells in ovarian follicles. The levels are quite constant and the AMH test can be done on any day of a woman’s cycle.
Since AMH is produced only in small ovarian follicles, blood levels of this substance have been used to attempt to measure the size of the pool of growing follicles in women.